You may have noticed a Leading Contributor badge in the footer of our website and wondered what it means. Chances are you haven’t heard of the Bariatric Surgery Registry (BSR), part of the Central Clinical School at Monash University. Upper GI Surgery has been awarded Leading Contributor to the BSR since 2016, recently being awarded our latest accolade for 2022. But what is the BSR?
The primary aim of the Bariatric Surgery Registry is to measure outcomes for patients undergoing bariatric surgery across public and private hospitals in Australia and New Zealand. It is predominantly a quality and safety registry. (Monash).
The BSR collects information on patient weight loss, change in diabetes status and problems related to the surgery, both in the short and long term. Contributing to the BSR is not compulsory, and it does take extra time and effort from medical teams to submit the information. So why is it so important?
What the BSR aims to do
The Bariatric Surgery Registry states that its aims are to:
Record the immediate safety of bariatric surgery in Australia – surgical safety & quality.
Study (longitudinally) the safety and efficacy of bariatric surgery in Australia (of) – procedures, devices, complications and re-operations.
Track key health changes following bariatric surgery in Australia – weight change & diabetes treatment.
This project is unique and important. It will provide us with an unprecedented tool for quality assurance. The outcomes of the Registry will provide hospitals, device manufacturers, government bodies and insurers with a greater understanding of the outcomes of bariatric surgery patients. It will provide a valuable resource to better understand and reduce factors associated with sub-optimal outcomes and improve surgical practices. (Monash).
What does this mean for our bariatric patients?
It means that a “second pair of eyes” looks at our outcomes and can act as an early warning system if unexpected or poor outcomes start occurring, even if they occur many years after the procedure. Audit is part of the “quality mindset” which is part of the drive towards excellence that not all surgeons share. It helps us compare our safety and weight-loss outcomes against others and allows us to report back to patients about what their outcomes may be. We are very happy to report that our audit results are very favourable.
Adverse outcomes after surgery
At our practice, 2.1% of bariatric patients have experienced a side-effect from surgery within the first 90 days vs the Aust/NZ average of 3.9%. The large majority of ours being re-admission for IV fluids, or the need for an endoscopy. Bleeding and leaks are under 1 in 500.
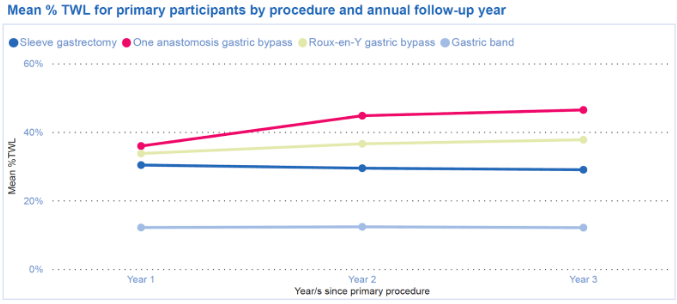
Weight loss after surgery
Total weight loss (TWL) results in our practice are also better than the Aust/NZ average.
Our sleeve gastrectomy patients lose 30% of their start weight (same as the Aust/NZ average).
Our one-anastomosis/mini gastric bypass patients lose 45% of their start weight vs the Aust/NZ average of 35%.
Our Roux Bypass patients lose 37% of their start weight vs the Aust/NZ average of 32%.
Come on Australia…and NZ
The BSR currently captures 75% of bariatric surgeries performed, but the aim is to get to 95%. Less than 2% of patients opt-out of the system, as most people value the idea that their de-identified data helps ensure the safety and effectiveness of what we do. This does mean however that there is a small subset of surgeons who don’t wish to have their outcomes and safety data compared against their peers which is a concern.
The most recent Bariatric Surgery Registry report (2022) lists a total of 115,234 participants; in Australia there are 181 surgeons and 121 hospitals contributing to the registry. Bariatric surgeons at Upper GI Surgery and St George Private Hospital contribute to the BSR each year, as resources like this help to influence changes in policy, and provide the highest safety and quality assurance for patients.
The message from the BSR Chair, Ian Caterson, called out those who are still choosing not to contribute to such an important system.
“Despite these impressive numbers and the work of our contributors, it is disappointing that there are still some hospitals and surgeons who have not embraced this enterprise and it is particularly disappointing when some public hospitals have decided to opt out of the Registry citing cost issues and time. Hopefully they will reconsider.”
By continuing to contribute annually to the BSR, committing valuable time and effort to do so, we are ultimately doing this to provide the highest quality of care and treatment available to our patients. Patients receiving obesity treatment at Upper GI Surgery can be confident that safety and quality assurance is our highest priority, alongside advocating to end stigma and make necessary societal changes.
“The surgeons, the staff in their rooms and in theatres, with their expertise and continuing interest and involvement have worked hard to provide data. The Registry can only be as good as the data it gets.”




0 Comments